Awake tracheal intubation
Web link: Open online
Zotero link: Open in Zotero
Tags: Difficult airway,
Abstract
Notes
Annotations
(8/6/2022, 7:10:57 PM)
“Awake tracheal intubation (ATI) is defined as successful placement of a tracheal tube in a patient who is awake and breathing spontaneously.” Go to annotation (Vora et al., 2022, p. 298)
“ATI is indicated in any patient with predictors of difficult tracheal intubation or face mask ventilation; these may stem from pre-existing patient factors or as a consequence of the presenting pathology.5 In cases of recognised difficult laryngoscopy and tracheal intubation, where facemask ventilation is possible, asleep techniques may be considered more appropriate, and it is useful to develop these skills for the management of the unpredicted difficult airway. Absolute contraindications to ATI are limited only to the patient’s refusal, despite appropriate explanation. Relative contraindications include: allergy to local anaesthetic, airway bleeding (where blood may obscure the image achieved through a flexible bronchoscope or videolaryngoscope), the uncooperative patient and certain airway tumours (with the potential to cause a ‘cork-in-bottle’ airway obstruction).” Go to annotation (Vora et al., 2022, p. 299)
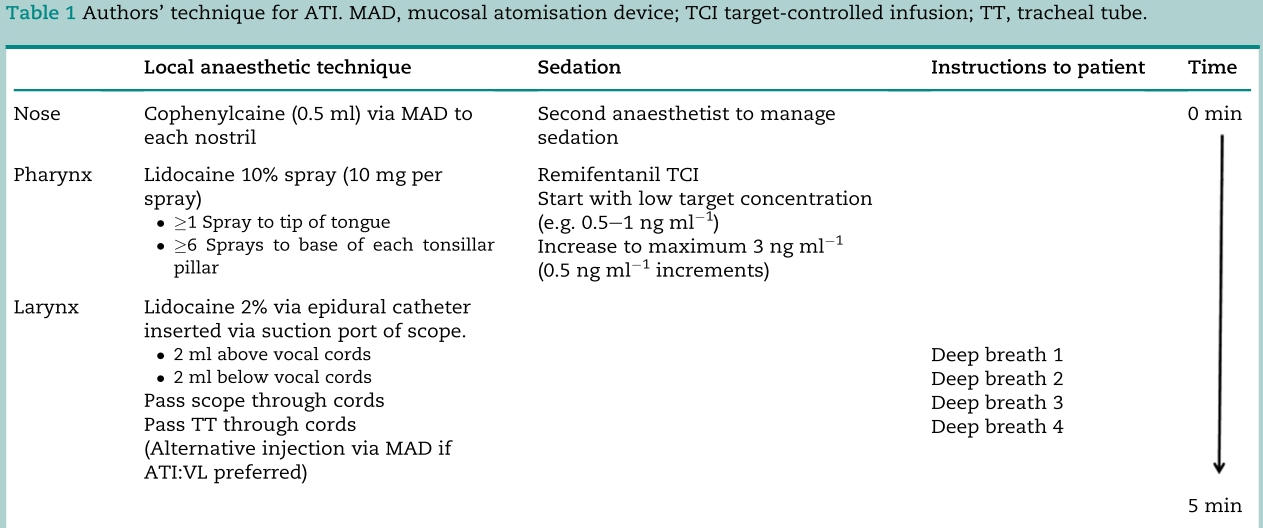
“Adequate airway topical anaesthesia is vital to the success of ATI approaches and lidocaine is commonly used for this purpose. It is available in a variety of pharmaceutical preparations, including combination with vasoconstrictors (such as adrenaline and phenylephrine) which reduce the likelihood of epistaxis when nasal intubation is preferred.2 The maximum prescribed dose for topical anaesthesia is 9 mg/kg, although in practice doses this high should not be required by those experienced in ATI. Cocaine has the advantage of intrinsic vasoconstrictor activity but concerns regarding its adverse cardiovascular effects mean its use is no longer recommended.” Go to annotation (Vora et al., 2022, p. 299)
“Antisialogogues reduce airway secretions, thereby improving airway anaesthesia and maximising the view achieved by a flexible bronchoscope. Options include the antimuscarinic agents glycopyrrolate, atropine or hyoscine. If used, glycopyrrolate 4 mg/kg i.m. should be given 40-60 min before performing ATI, for peak mucosal drying effect. The tachycardia associated with antimuscarinic agents may increase the patient’s anxiety and hinder ATI, and their use is therefore not considered mandatory.” Go to annotation (Vora et al., 2022, p. 302)
“Remifentanil is a potent mu-opioid receptor agonist. It is rapidly hydrolysed by non-specific tissue and plasma esterases responsible for its rapid offset in action and therefore ease in titration. It is an analgesic and antitussive agent that can be used as the single sedative agent during ATI. It may be used alone in the rare cases where topicalisation is contraindicated. Recent guidelines advocate its use at effect site concentrations of 1.0-3.0 ng/ml. It is associated with high rates of patients’ satisfaction, but the incidence of recall is higher when remifentanil is used as the sole agent.17 Adverse effects of remifentanil relevant to ATI include: bradycardia, hypotension, apnoea, hypoxia and chest wall rigidity.” Go to annotation (Vora et al., 2022, p. 302)
“Dexmedetomidine is an agent with a-adrenoreceptor agonist activity with a markedly increased affinity for a2 over a1 adrenoreceptors in comparison with clonidine. Effects upon a2-adrenoreceptors within the pons mediate its sedative effects, whereas action at spinal a2-adrenoreceptors produces analgesia. Its ability to produce sedation and analgesia without respiratory depression means it is becoming increasingly used for procedural sedation including ATI, although this is currently an unlicensed use in the UK. The cardiovascular effects of a2-agonists are an important consideration. Inhibition of noradrenaline release and bradycardia reduce cardiac output and result in hypotension.18 Direct effects on vascular tissues after the injection of i.v. bolus doses may result in the development of transient hypertension, causing further reflex bradycardia.17 Doses are as follows:
- a loading dose 1 mg/kg given over 10-20 min followed by
- infusion starting at 0.7 mg/kg/h
- titrated to the desired clinical effect at between 0.2 and 1.0 mg/kg/h.
At the time of writing, no target controlled infusion (TCI) model exists. The long duration of bolus dose required is potentially problematic when ATI needs to be performed urgently.” Go to annotation (Vora et al., 2022, p. 302)
“An unsuccessful attempt at ATI is defined as unplanned removal of the flexible bronchoscope, videolaryngoscope or tracheal tube from the airway.2 Repeated unsuccessful attempts at ATI increase the likelihood of airway bleeding, obstruction and further difficulty.” Go to annotation (Vora et al., 2022, p. 303)